What is the knee joint?
The knee joint is the mobile connection between the thigh bone (femur) and the shin bone (tibia). Cartilage lines the knee joint, and the moving surfaces are held together by strong ligaments and tendons. The knee works roughly as a hinge joint, although ac-tual knee movement and geometry are far more com-plex than a simple hinge. Knee motion involves rota-tion, sliding, and many other types of movement.
How does the normal knee joint get lubricated?
The joint lining (called synovium) secretes a grease-like liquid called synovial fluid, which reduces friction in the knee joint. This fluid is produced in other joints also, and it is the equivalent of biological “motor oil.” This oil-like fluid keeps the knee joint lubricated.
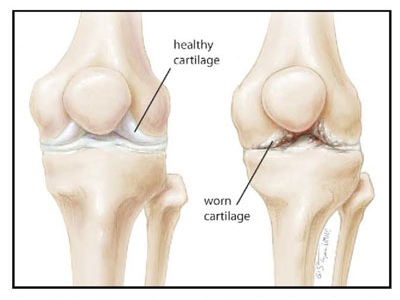
What is a degenerative knee joint?
As cartilage gets rough, the friction in the joint increas-es. The result is an inflamed knee joint that swells and hurts. Arthritis and injury are usually responsible for degenerative changes in the knee. Pain, leg deformity, and disability can get severe enough so that patients seek help.
Why does cartilage get damaged?
Cartilage can be damaged by injuries, overuse, inflam-matory conditions (like gout, rheumatoid arthritis, and others), and genetic causes. Obesity, poor joint alignment, age, and repetitive trauma to a joint can also damage cartilage. Diseased cartilage loses its smooth, friction-reducing surface, leading to progressive roughening of this biological bearing.
What causes the painful and annoying symptoms of arthritis?
When bone touches bone in the knee joint after loss of cartilage, the result is pain, grinding, swelling, and stiffness. The pain comes from inflammation in the tissues lin-ing the knee joint; inflammation comes from abnormal movement and friction. This is why anti-inflammatory medicines such as aspirin and ibuprofen can often help arthritic pain, at least early in the disease. Swelling and fluid on the knee are adaptive mecha-nisms by which the body tries to deal with an inflamed and arthritic knee joint.
Is the wear of knee cartilage inevitable with old age?
Not particularly. Even though everything wears with time, the knee joint wears differently from person to person. Most people will never need knee surgery re-gardless of age. Others are at increased risk of develop-ing arthritis. While family history, racial origin, and genes may play a role in this, there are things you can do to manage an arthritic knee. Establishing a routine of light aerobic exercise, maintaining ideal body weight, and avoiding extreme sports that injure the knee are some steps that will help reduce the risk of wear in the knee.
How is worn cartilage diagnosed?
Symptoms such as pain, swelling, stiffness, lack of movement, and grinding in the knee can suggest that knee cartilage is no longer smooth. X-rays are a com-mon way of diagnosing diseased cartilage in the knee. The X-rays show the bones around the joint. The carti-lage layer cannot be seen on X-rays, and shows up as a space between the femur and tibia bones.
In a healthy knee, this space is about a quarter of an inch thick. When joint space taken up by cartilage is destroyed by arthritis, X-rays will show joint-space nar-rowing. With significant cartilage loss, the bones may touch each other; doctors call this finding “bone-on-bone” on the X-rays. Over time, cysts and bone spurs may form around the knee. Left untreated, the leg can get so deformed that it appears to be either bow-legged or knock-kneed.
Are there other ways to see the extent of damage to knee cartilage?
MRI scans are a special X-ray study that can diagnose diseased cartilage somewhat more accurately and at an earlier point than plain X-rays.Another method includes actually looking inside the knee during a procedure called “knee arthroscopy.” This involves the surgeon placing a small camera in the knee and inspecting the cartilage. We have a separate book, in print and on our website, describing knee ar-throscopy in specific detail.
Treatment Options for Arthritis of the Knee
Does exercise help arthritic knees?
Yes. Exercises to stretch and strengthen the quadriceps muscles and hamstrings are helpful in reducing the pain of arthritis. Stronger muscles and weight loss will decrease the mechanical loading of the knee joint, re-sulting in pain relief. Walking, jogging, swimming, light aerobics, elliptical exercisers, and other related activities can be very use-ful. In some patients, a physical therapist can help de-sign an exercise program to help an arthritic knee. Any exercise is far better than no exercise. Exercise will not make arthritis worse, and will not accelerate the wear and tear in the knee.
Does weight loss help with knee arthritis?
Yes. Excess body weight is multiplied across the knee joint. Thus, gaining 10 pounds of body weight can lead to a 30-pound load on the kneecap, making getting up, climbing stairs, and squatting very difficult.
Losing weight takes load off the cartilage, and decreas-es the burden on your knees. Weight loss also makes surgery safer. Generally speaking, weight loss and the maintenance of proper body weight can help reduce the pain of knee arthritis.
Does using a cane help with knee arthritis?
Yes, it does. Similarly, using a walker or other assistive device can help by off-loading the knee joint and re-ducing the tendency to limp. Most people would rath-er not use a cane, but using one will help with the pain of an arthritic knee.
Will a brace help with knee arthritis?
It depends. Over-the-counter knee braces can be very effective at controlling pain and giving you more con-fidence and balance in the knee. More expensive cus-
tom braces are rarely necessary. Wrapping the knee with an elastic bandage can also relieve arthritic pain.
What other non-surgical steps can I take to relieve pain of knee arthritis?
When possible, avoid stairs and concrete floors, lift-ing weight, deep bending, twisting activities such as golf, and repetitive impact such as jogging. These are all reasonable, non-surgical options that people use to relieve the pain of an arthritic knee until they are ready for surgery.
Will alternative therapies like supplements and acupuncture help?
Some patients find relief by using over-the-counter remedies like glucosamine, vitamins, oils, shark car-tilage, herbal supplements, etc. Such remedies often lack scientific proof of their beneficial effects; be sure to read and understand the package label.Chiropractor manipulations, acupuncture, massage, heat packs, prolotherapy, aqua-therapy, and related alternatives may also help. Explore and use these op-tions if you feel they are of value. Of course, you should stop any therapy or manipulation that increases your pain.One important note: If you are scheduled for surgery, stop all herbal, vitamin, and alternative medications at least 10 days before surgery, to avoid excess bleeding and interactions with anesthetics.
Do knee injections help?
Cortisone injections placed in the knee joint can pro-vide relief; the duration of relief varies from patient to patient, often depending on how worn out the knee is. Most patients will get a month or so of relief after a cor-tisone injection; others may get longer-lasting relief. Lubricant injections can be given weekly over three to five weeks; these replace the normal knee lubricants. Modern versions of these injections allow for one in-jection that is given every three to six months or so. For arthritis that is not quite bone-on-bone yet, these injections can help, and allow patients to enjoy life without having the knee replaced.
How long can I rely on medication as treatment for my arthritic knee?
It depends. Anti-inflammatory medications such as as-pirin, ibuprofen, and others in this class of drugs are not addictive drugs. As long as your primary physi-cian is aware and monitors your kidney function, these medications can be taken, within the safe dose range, for many years, even on a regular basis.
Alternative medicines such as glucosamine chondroi-tin might also help with knee pain. These medicines may not work for everyone, but they are worth a try; in some cases, they can help considerably.
Narcotic drugs are more risky and can create depen-dence. Also, long-term use of narcotics before surgery makes pain control after surgery more difficult. If your knee pain has progressed to the point where you re-quire narcotic medication, it may be time to think about surgery.
Why not just replace my knee instead of trying non-surgical treatments?
Surgery should be the last option. No knee operation can ever restore the complexity and superior function of your own knee. Surgery also has risks. Experience shows that patients who wait and exhaust all other op-tions before knee surgery have the best outcomes.Those who rush into surgery without all the informa-tion are often unhappy afterward. That is why any responsible surgeon will work with you to try all non-surgical options first. Never rush to surgery, and never bypass other methods of obtaining pain relief.
Does arthroscopic surgery help in the treatment of knee arthritis?
For some patients, yes. Knee arthroscopy can help by providing several years of pain relief. Such cases usu-ally involve early knee arthritis that has caused a car-tilage tear.Arthroscopy is an outpatient surgery where two or three holes are made in the knee for a camera and in-struments that can remove arthritic debris, loose piec-es, tears, and related pathology. Sometimes, injections and physical therapy are necessary after knee arthros-copy. The key value of arthroscopy, in selected cases, is the ability of the surgeon to get a first-hand view inside the joint. This information is not usually available by other methods, and can be useful in planning treatment and understanding the prognosis. If the cartilage destruction is severe, however, ar-throscopic surgery is unlikely to help, and a knee re-placement may be indicated. More details about ar-throscopy are contained in a related guide.
Are there non-implant surgical options to treat arthritic knees?
In young patients with non-inflammatory arthritis of the knee joint that is not yet extensive and in whom leg deformity is significant, an osteotomy can be done to realign the leg. This procedure involves cutting bone and realigning the axis of the leg, similar to wheel alignment in a car, to take off the wear from inside or outside the tires. Only a few patients are candidates for such joint-con-serving procedures, and we can advise you if you are such a candidate.
When should knee replacement be considered?
The right time to consider knee replacement is when pain pills, exercise, weight loss, bracing, ice, heat, injec-tions, and various alternative therapies no longer pro-vide sufficient relief from the pain of an arthritic knee. Knee replacement offers dramatic pain relief and in-creased motion. Some soreness and stiffness will per-sist for weeks to months in a few patients, but ultimate-ly most people are glad they had surgery. If pain, swelling, grinding, deformity of the leg, and decreased ability to function are severe enough to get your attention, and non-surgical options have not worked, it may be time to consider replacement surgery.
Knee Replacement Surgery Basics
Is knee arthroplasty different from knee replacement?
No. The terms can be used interchangeably. Total knee replacement is also called total knee arthroplasty. Simi-larly, a partial knee replacement is called uni-compart-mental knee arthroplasty.
Is knee replacement surgery a fairly routine operation?
Yes. Hundreds of thousands of knees are replaced each year in the U.S., and world demand for knee replace-ments is increasing as people live longer and want more out of their lives. In our practice, we perform hun-dreds of knee replacements each year. While routine, knee replacement is still serious surgery. Each patient is unique, and each person’s anatomy demands care-ful attention to detail and precise steps during surgery.
Will a new knee joint be a perfect substi-tute for the real knee?
No, and you should be skeptical of any doctor or adver-tisement telling you otherwise. Those advertisements are designed to make a sale, rather than educate and enlighten consumers. Normal human knee movement consists of gliding, rotation, sliding, and other complex movements. A synthetic joint can only approximate the intricacy and complexity of the knee joint that you were born with. No artificial knee joint, regardless of manufacturer’s ad-vertising claims, or surgeon claims, has ever duplicated the complexity and intricate movements of the natural human knee. The human knee joint has major ligaments and other soft tissue supports; these have fine nerve endings that send sensory, positional, and perceptual feedback to the brain from the knee. An artificial knee is simply metal and plastic. For severely diseased knees, modern total knee replacements provide excellent pain relief and function, but they are never a perfect substitute for the real thing.
What does an artificial knee feel like, if it does not feel natural?
Replacing your natural knee joint is a bit like replacing your natural teeth with dentures. Your own teeth are more than mechanical devices; they play a complex role in biting, chewing, hot-cold sensation, positional sense, vibration, and even taste. Dentures are not natural or normal; they lack nerve endings and cannot feel vibration, heat, cold, touch, or any of the things we take for granted with our natural teeth. That is why dentures are useful only for patients whose own teeth are decayed or destroyed. Similarly, knee replacements are useful for patients with severe cartilage destruction, who have no other options, and who have thoroughly explored all their options.
How can I increase my chances of a success-ful knee replacement?
The success of knee surgery depends on your partici-pation and how your body heals. Any operation on the human body has some uncertainty with respect to the outcome, despite the best of care. Healing is a complex process, and each person heals differently. It has been our experience that knowledge and a strong partnership between us leads to greater success, and also allows us to work through any un-expected outcomes. The purpose of this guide is to bridge the information gap; to tell you what we know from experience; and to encourage communication.
Can arthritis occur in a knee that is re-placed?
No. Since cartilage is replaced by metal and plastic dur-ing knee replacement, there is no cartilage left in the knee to deteriorate. However, arthritis is a complex dis-ease that frequently affects surrounding tissues, such as muscles, nerves, ligaments, and the synovial lining of the joint. This is one reason why despite a successful knee replacement, some pain, stiffness, and swelling may persist for many months. In some patients, arthritis in other joints, such as the back and hip, can contribute to continuing symptoms after surgery. This is an important point to understand. Not all knee pain is from the knee; some may be com-ing from a diseased hip or spine, or other systemic ill-ness like fibromyalgia or rheumatoid arthritis. Stiff muscles, tendons, and ligaments can take many months to return to normal, even after healing from a knee replacement.
How long is the recovery after a total knee replacement?
Most patients are happy, mobile, and about 70 to 80 percent recovered by one month. Individual medical conditions such as diabetes, smoking, advanced age, obesity, neuropathy, heart and lung disease, Parkin-son’s disease, and related variables can change recov-ery time drastically. About 80 to 90 percent of the recovery is complete by six to eight weeks, but some aches and stiffness can persist for many months. The last 5 percent to 10 per-cent of soreness, achiness, and stiffness can take a year or two to subside completely. For most patients, the most significant part of the re-covery takes place during the first month. But keep in mind that patient variability is great; there is no value in comparing yourself with anyone else. Each person has a unique recovery.
Is recovery from knee surgery faster for younger patients?
No, and you should know about this paradox. Experi-ence shows that the best recovery from knee replace-ment is in older patients, who have severe arthritis, and who have tried all reasonable conservative means of treating pain before surgery. Younger patients, especially those of male gender and muscular physique, generally tend to have a notice-ably slower recovery and higher level of pain from any knee surgery. This may reflect different expectations, different pain tolerances, body image, hypersensitiv-ity of younger tissues, and other variables, but it is a fact that the younger patient should approach knee replacement surgery with added caution.
What is the best age for knee replacement surgery?
The optimal range is late 50s to late 70s. Most knee ar-thritis affects this age group, and a properly implanted total knee replacement should last the rest of life in such patients.
Should I get a second opinion before knee surgery?
Yes. If you have unanswered questions or doubts, ad-ditional opinions are always a good idea. A wealth of information exists on reputable websites. You can also learn a lot from orthopaedic implant companies as well as from friends, family, and others who have had knee surgery. It is best to explore all your options and make your de-cision accordingly. Treat all information with a healthy dose of skepticism; any credible resource should be able to answer your questions to your satisfaction, no matter how authoritative or influential that resource holds itself to be.
A surgeon replaced my knee, and it did not work well. Can anything be done?
Usually, yes. Knee replacement surgery can be compli-cated by subtle infection, implant malpositioning, and other unexpected outcomes that can leave patients unhappy. If this is the case, you should always seek a second opinion, even if a doctor has told you that nothing can be done. We have been able to help many people who had a poor result after a knee replacement done elsewhere, and who were told to live with it. A variety of complex factors can compromise the results of knee replacements; fortunately, most such problems can be fixed effectively.
What are the risks of knee surgery?
Knee surgery, regardless of technique, has a small risk of infection, nerve injury, deep blood clots, premature implant loosening and failure, unexpected knee stiff-ness, continued pain, and unpredictable complica-tions, which can even include death. There is no hospi-tal, doctor, or surgical technique in the world that can claim to have reduced the risk of these adverse out-comes to zero. Be suspicious of any surgeon or hospital that claims otherwise, and seek treatment elsewhere.Complications are very rare, but patients planning any surgery should know about them, and take the time to understand them. Note: You will find a comprehensive listing of complications and a detailed discussion at www.hipandknee.com. If you are unable to access this site, Dr. Bal and his staff will provide this information.
How much does a total knee cost?
It is hard to give an answer since insurance contracts, hospital pricing, medical billing, and other variables related to cost are very complex. If you want to know the costs involved, please contact our office and a member of our staff will be glad to assist you.
Will Medicare or my insurance cover my surgery and therapy?
Each insurance plan is different, and benefits can vary and change over time. To get information on your plan’s coverage please check with your insurance com-pany or contact our office with your insurance informa-tion. Rest assured, we always obtain pre -authorization for any surgery and hospital stay. Many patients have traveled from other states and outside our geographic area to have surgery; many insurance companies will allow such travel for treatment.
Types of Knee Replacement Surgeries
What is a “total knee” replacement?
Total knee replacement is a surgical procedure that removes all (hence, “total”) diseased joint surfaces in the knee, and replaces them with artificial surfaces. These artificial surfaces are metal alloys based on co-balt-chromium and titanium metals. Some total knee designs used overseas are made of ceramics; such de-signs are not used widely in the United States.Actual movement of an artificial knee is between a very smooth, polished cobalt-chrome metal, contoured like your own knee, and a low-wear plastic bearing that sits inside a titanium tray designed to attach to bone. Liga-ments inside the knee joint are removed, while liga-ments supporting the knee on the outside are usually preserved. A total knee replacement provides all new weight-bearing surfaces in the knee joint. It serves to decrease pain and increase motion in the joint since the synthetic metal and plastic surfaces do not have any nerves.
What is a “partial” knee replacement?
Total knee replacement involves all three compart-ments (or sub-joints) in human knee joints. Usually all three compartments are all worn out by arthritis, but in some knees, only one or two compartments may be arthritic. If so, the affected compartments can be re-placed selectively, thereby preserving bone and mini-mizing surgery. Such knee replacements are called partial knee replacements.Very few patients are proper candidates for partial re-placements, despite the marketing claims of surgeons and manufacturers. If a partial replacement is done improperly, or in the wrong patient, premature repeat surgery is usually needed to put in a complete knee prosthesis, which likely should have been used in the first place.
Is recovery faster after a partial knee replacement?
Yes, in part, because all the knee ligaments (anterior cruciate ligament and posterior cruciate ligament) are preserved in all partial knee replacements. These liga-ments are removed during a total knee replacement. Newer knee implant systems now allow selective re-placement of one or more arthritic compartments in the knee, thereby customizing the amount of surgery to each patient, and ensuring even faster recoveries. In these selective compartmental replacements, liga-ment preservation leads to earlier recovery, a more natural feeling joint after surgery, and less blood loss and surgical trauma. Still, keep in mind that for most patients, a total knee replacement is usually the most durable and satisfactory option.
What is “minimally invasive” knee replace-ment?
The term “minimally invasive” is misleading, over-used, and abused. Many hospitals, companies, and doctors use the term simply as a means of attracting patients in today’s competitive health care environment. For many community surgeons, minimally invasive sur-gery means doing the same old operation through a shorter skin cut. Minimally invasive or not, you should know that all surgery is inherently invasive. The response to surgery includes discomfort, altered emotions, nausea, altered appetite, constipation, and other unpredictable sen-sations. It takes time for the body, soul, and mind to heal. Other conditions such as diabetes, heart disease, smoking, stress, obesity, and lack of family support can prolong recovery after any surgery.
How does your practice define “minimally invasive” surgery?
In our practice, minimally invasive knee surgery re-flects a comprehensive treatment program involving the latest implants, better instrumentation, smaller incisions, improved anesthetic techniques, earlier re-habilitation, altered pain management techniques, en-hanced patient communication, a team approach, sur-gical efficiency, and new surgical methods that reduce or eliminate trauma to muscles and tendons.Our minimally invasive surgery program is a compre-hensive and continually improving collaborative effort to bring together the latest technologies and tech-niques from the best surgeons worldwide. This effort is always progressing and improving, for every member of our team. We also recognize that minimally invasive surgery can reduce, but cannot eliminate the normal physiologic and psychological responses inherent to surgical trauma.
Parts and Materials Used for Knee Replacement
Are there different kinds of knee implants?
Yes. There are several different types of knee replace-ments. All of them are variations of the basic design introduced more than 30 years ago, which is called the “total condylar posterior stabilized knee.” The choice of implants depends on factors such as the status of ligaments and the amount of deformity in the knee. Usually, we use a “high-flex” design that is safe for deep knee bending. The implants come in “gender-specific” versions engineered to match the knee anatomy of men and women. As new designs in total knee replace-ments are developed, we will adopt them in our prac-tice only after carefully considering the advantages, safety, and scientific merits of such designs.
Can you show me the parts used in a total knee replacement?
Yes. In addition to the figures shown in this book, we have actual parts in the clinic that you can see and hold, as well as videos and animations on our website, www.hipandknee.com
What brand of knee implants do you use?
We generally use implants made by Zimmer. You can learn more about the company by visiting www.zim-mer.com. The company also has patient-specific infor-mation at www.pacewithlife.com. There is very little difference between the implants offered by the major manufacturers, even though each one will claim to be the best. (Note: Neither Zimmer, nor any other implant company pays Dr. Bal to promote or implant its prod-ucts and no commercial entity has contributed, in any way, to the preparation of this guide.)
What if I want a different brand of knee prosthesis?
New implants are sometimes hyped up by local sur-geons and hospitals eager to get your business. Some of these newer designs are true improvements, while others are simply old designs with new packaging, gimmicks, and slick marketing. As a new design is in-troduced and marketed by the orthopaedic implant industry, we will present it with an unbiased discussion on our website, www.hipandknee.com. If truly inno-vative implants are introduced, the odds are that we have been using them well before they are released to community orthopaedic surgeons. If you have an inter-est or preference for a particular type or brand of knee implant, please let us know and we will explore the op-tion together.
Can ceramic parts be used in knee replace-ments?
Yes. The advantage is the lower wear rate of ceramics when compared to metals. In the United States, ceram-ic knees are used on a limited basis since the Food and Drug Administration (FDA) has not approved them for general use. Several years ago, we conducted one of the few clinical trials in the country on ceramic knees. Ceramic parts are useful in the rare cases of a true met-al allergy in selected patients. Ceramic components will likely become more common in the future. At the time, ceramic materials in total knees are more com-mon overseas. Balancing the very low wear rates of ce-ramics is the fact that we do not have enough scientific data from U.S. studies to support their routine use in total knee replacements as of yet.
Do you use the same model of knee im-plant for all knee replacements?
No. Each patient situation is unique, and the type of implant chosen depends on many patient variables, including age, gender, weight, bone dimensions, liga-ment condition, bone quality, anticipated activity level, and occupational history.In older patients with weak and osteoporotic bone, for example, the best choice may be a cemented model supplemented by design features that will support ex-ternal knee ligaments. On the other hand, for a healthy young person with physically demanding job, the ideal model may be an uncemented total knee design that allows as much bone preservation as possible.In patients who have had knee replacement in the past and are in need of repeat surgery, it is often necessary to use more complex models, to reconstruct deficient and missing bone.
Are newer knee implants much different from old ones?
Yes. There are newer “high-flex” knee designs that al-low greater safety during deep knee bending. There are also newer “gender-specific” total knees made to fit the anatomical differences in the knees of men and women. All knee replacement components that we use incorporate these modern design features. As newer designs evolve and are approved by the FDA, we offer them to our patients. Other variations in total knee implants include a ceramic “oxinium” surface, the “rotating-platform” knee, and other brands marketed by implant companies. Let us know if you have a pref-erence, and we will help you make an informed choice.
Can I get a “golfer’s knee” implant?
As above, if you prefer one kind of implant over the other, we can discuss the options. Keep in mind that no knee implant is better suited for golf or any other sport. Participation in activities such as golf is equally possible, and equally easy with any of the competing knee designs out there, whether or not they claim to be a “golfer’s knee.”
What about a custom knee replacement, made from CT/MRI studies?
Almost all companies making total knee implants are now promoting the so- called “custom knees,” where the vendor either makes an implant that is customized to your anatomy, or creates specialty alignment instru-ments made just for your body.
At present, there is no evidence that such custom knees are necessary, and such devices add the need for an additional CT scan or MRI study to knee replace-ment surgery. Knee replacement is a multi-step pro-cedure requiring expert evaluation and assessment of tissue-tension, ligament balance, and a “feel” that comes through years of experience. An experienced surgeon’s brain, eyes, sense of touch, feel, judgment, and surgical intuition are the best customizing pos-sible. Knee replacement components come in a large variety of sizes, options, designs, and configurations sufficient to fit nearly any patient.
Very rarely, in patients with congenital dwarfism or gi-gantism, where body sizes are unusually small or large, or in cases of a true metal allergy, a custom prosthe-sis might be necessary. For all other patients, custom products do not offer any incremental benefit at this time.
Are there other implants that are used to treat knee arthritis?
In unusual cases of knee arthritis and in relatively young patients, a shim-like device called the uni-spac-er may be used. This device acts like a spacer to sepa-rate the worn-out knee surfaces and keep them from grinding against each other. Very few patients meet the criteria for this type of surgery, and a uni-spacer is a temporary option, best reserved for very young pa-tients with knee arthritis.
In what cases do you use human tissue for knee replacement?
In rare cases, we use cadaver tissue for reconstruction of the extensor mechanism in selected knees. These are complex cases with previous trauma that has rup-tured the quadriceps tendon in addition to causing arthritis of the knee. For the majority of knee replace-ments, no human tissue is ever needed.
How does the artificial knee joint get lubri-cated?
After a joint replacement, the artificial bearing gets its lubrication from synovial fluid, just like the natural knee joint. After surgery, the synovial lining re-forms and secretes synovial fluid. In cars, oil must be changed regularly, but in the body, synovial fluid is recycled by the cells. No external lubrication of the knee joint is ever necessary. In fact, any injections placed into your artificial knee joint increase the risk of infection.
Can patients become allergic to the knee replacement parts?
The metals used in artificial knees are alloys of cobalt- chromium and titanium. The bearing portion of the joint is made of a high-grade, wear-resistant plastic. The metal-plastic bearing combination is the most common type used in knee replacement implants worldwide. These metals have been used in humans for many decades and millions of patients with very successful results. Allergic reaction to artificial knee parts is virtually unheard of, and is not a routine clinical concern.
What actually moves inside an artificial knee joint?
In an artificial knee joint, highly polished cobalt-chromium metal moves against a very durable plastic spacer to allow movement. This bearing is lubricated by your body’s own synovial fluid, which is constantly replenished by living cells. The power to move the ar-tificial knee, once implanted in your body, comes from your own muscles. That is why the condition of your muscles affects how quickly you recover after any type of knee surgery, including a total knee replacement.
Techniques Used During Knee Replacement
How do you attach the artificial knee to my bone?
We use bone cement to do this. The majority of total knees are affixed with cement, although un-cemented designs are also used. Outcomes from both are very good. For young and active patients, cement-less total knees are usually preferred because of excellent fixa-tion and durability. Living bone next to the prosthesis keeps the implants secured over time, whether or not cement is used. The choice of cemented versus un-cemented knee depends on many factors, such as pa-tient age, knee deformity, status of ligaments, and the quality of bone.
Who does the actual surgery?
Although team members will assist, and resident phy-sician or students may observe, rest assured that I will perform the entire operation.
Do you replace my kneecap too?
In part, yes. On the underside your own kneecap (also called the patella) a thin layer of arthritic cartilage and bone is removed during surgery. In its place, we affix a plastic kneecap to your own remaining kneecap. This new part functions just like your own kneecap. The front surface of the kneecap is your own bone; it is the underside of the kneecap that is lined with plastic.
Are knee ligaments removed during surgery?
Internal knee ligaments (anterior cruciate ligament and posterior cruciate ligament) are usually so worn out in arthritic knees that what remains of them is removed. The knee prosthesis itself is engineered to substitute for internal knee ligaments and stabilize the joint.
The supporting ligaments outside the knee joint are usually preserved during replacement surgery. These external ligaments are called the medial collateral liga-ment (located to the inside the knee) and the lateral collateral ligament (located to the outside of the knee). These ligaments continue to function after knee re-placement surgery. For severe deformity, arthritic de-struction, or unusual cases, we use prosthetic designs that can substitute for all knee ligaments, providing more stability when compared to routine total knee prosthesis.
Thus, even very unstable and deformed knee joints can be replaced successfully, allowing the patient to fully weight-bear immediately, without fear of the knee giv-ing out, and without knee braces. The choice of im-plant is based on the individual case and amount of knee joint deformity, as well as surgical judgment.
Will my leg have a tourniquet on during surgery?
No. A thigh tourniquet is a device like a blood pressure cuff. It is placed on your thigh and inflated to let the surgeon operate easier, but cutting off the blood sup-ply to the leg while the knee joint is open. Tourniquets lead to increased tissue trauma to the thigh muscles, which are squeezed hard for the entire duration of sur-gery, and a lack of oxygen to the entire leg during the operation. The result is pain, tissue damage, and de-layed recovery.
We do not use a tourniquet on any knee operation, no matter how complex the operation. Keep in mind that for convenience and out of habit, most surgeons in the United States do use a tourniquet for knee replace-ment surgery though, so our practice is very different in this regard.
Will the knee bleed more without a tourni-quet?
Studies have shown no difference in blood loss during knee surgery done with or without a thigh tourniquet. Without a tourniquet, most blood loss occurs during the operation. If need be, this blood can be collected by a cell-saver device and given back to the patient. With a tourniquet squeezing the thigh, all the blood loss occurs after the tourniquet is let down and oxy-gen-deprived tissues get the blood flow restored. This blood is usually collected in a drain placed in the knee joint after surgery and discarded.Given these considerations, our practice is to avoid damaging muscles and other soft tissues by not using a tourniquet to choke off the blood supply to the leg during knee replacement surgery. Our patients recover faster, in part because of this practice.
How does computer navigation help in knee replacement surgery?
Precise alignment of the bones during knee replace-ment is critical to the long-term performance of the joint replacement. Computer programs can help in such alignment of bones, and reduce the possibility of error. Beyond computer-assisted technology, robotic arms help position bone preparation guides very pre-cisely, and optimize the result for each patient.
Robotic technology may someday take surgery be-yond the limits of the human hand, introducing pre-cise, versatile instrument movement combined with three-dimensional visualization of the operative site.
We investigate every new technology as it emerges, and so far, nothing seems to replace or substitute the skill and judgment of an experienced surgeon. At pres-ent, we do not use computer navigation and robotics routinely, since there is no advantage to these in our high-volume, sub-specialized practice.
Before Surgery
What do I need to do to prepare for knee surgery?
Reading this guide, communicating with your surgi-cal team, and paying close attention to the checklists at the end of this guide will best help you prepare for knee replacement surgery. The importance of prepa-ration and information to successful surgery cannot be overemphasized.
Health